Клініка репродуктивної медицини IVMED > Determination of ploidy of testicular biopsy cells
Today, about 20% of couples of reproductive age face fertility problems. The male factor of infertility accounts for about 50% of all cases.
The initial stage of male reproductive function assessment is the analysis of ejaculate - spermogram.
An example of a spermogram protocol
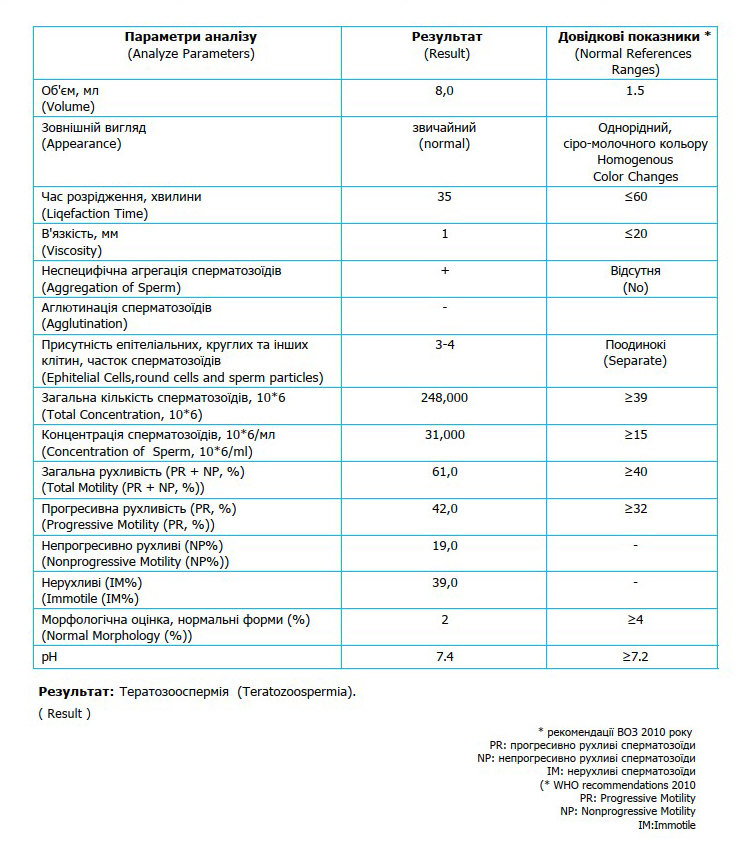
With the help of a spermogram, it is possible to detect deviations in the quantitative and qualitative indicators of sperm. However, in 15% of cases, andrology laboratory specialists are unable to find sperm in the ejaculate. This phenomenon is called azoospermia.
Azoospermia can be of two types:
1. Obstructive
2. Non-obstructive
Obstructive azoospermia in most cases is associated with problems of blockage of the vas deferens or ejaculatory dysfunction. That is, sperm formation occurs, but their excretion during ejaculation is impaired.
Non-obstructive azoospermia can be caused by hormonal disorders, structural features of the genital appendages, genetic and chromosomal abnormalities, and varicocele. That is, there is a violation of the process of spermatogenesis (sperm formation).
Spermatogenesis is the process of development of male germ cells (spermatozoa). As a result of two consecutive meiotic divisions, spermatogonia form haloid cells - spermatids, which, after passing the formation period, become spermatozoa.
Schematic representation of spermatogenesis
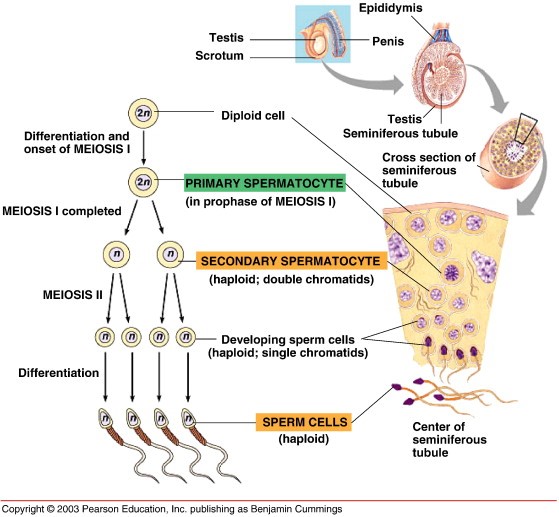
In such cases, patients are offered to undergo a TESE (testicular extraction of spermatozoa) or PESA (puncture of the epididymis) procedure. After this procedure, patients with obstructive azoospermia have a very high chance of obtaining spermatocytes and spermatids (sperm precursor cells with a haploid set of chromosomes) for further use in ICSI processes. They have a characteristic elongated shape and are visually distinguishable from spermatogonia (round cells with a diploid set of chromosomes) when microscopy of the sample is performed.
When performing TESE/PESA procedures in patients with non-obstructive azoospermia, microscopic examination of the biopsy is often ineffective, because the morphology of the cells obtained is almost identical, which means that it is impossible to clearly determine the ratio of haploid and diploid sperm precursor cells.
In such cases, it is recommended to examine the cells of the testicular biopsy/ epididymis for ploidy using the FISH method. This molecular cytogenetic analysis helps to determine the ratio of cells with haploid and diploid karyotype.
Photographs of FISH analysis of sperm progenitor cells using the fluorescent dye DAPI, a component of Metasystems AneuScore I prenatal commercial DNA probes; green signals are for chromosome 13, orange signals are for chromosome 21 (Lucia FISH software).

The results of this study help to predict the efficiency of using the obtained sperm progenitor cells in the processes of ICSI PROCESSES and enable the reproductive physician to select the optimal patient management plan.
Leave your contact information and our consultant will call you back and select the most convenient time, date, and doctor for a visit or online consultation.
Diagnostic tests, the choice of treatment, medications, programs - everything is adapted to your individual indicators and circumstances.
The clinic has been registered with the US Food and Drug Administration (FDA)
The clinic is certified according to the international quality management standard ISO 9001: 2015.
IVF-ID. Ukraine's first electronic system for protecting patient data and biological material.
By clicking, you accept the terms and conditions
“Consent to the collection and processing of personal data”